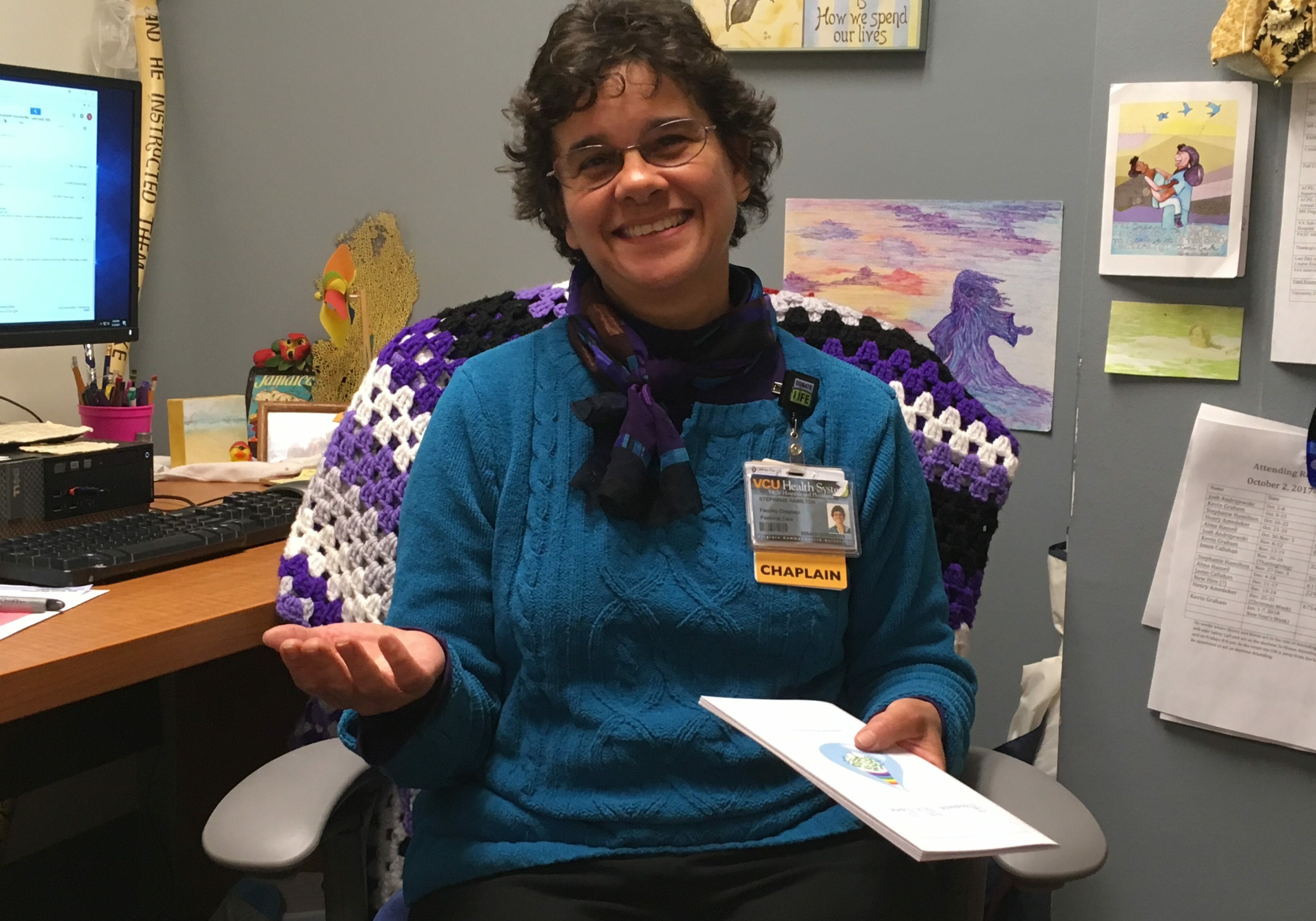
Life and Death through the Eyes of a Hospital Chaplain
Sometimes the miracle you get isn’t the miracle you asked for.
That’s a truth Stephanie Hamilton often discusses with families in her role as a family communication coordinator and head of bereavement services at VCU Medical Center.
When a family has been praying for a miracle – that their loved one will wake up and recover – it’s a profound moment when they realize that it isn’t going to happen.
Stephanie is often on hand to share their grief, talk them through it and counsel them in their anger, stress and sorrow.
“The miracle isn’t that my loved one is going to wake up and come back to life again. The miracle is that they will help someone else to do that and not die.”
“They’ve been hoping and praying that their loved one will wake up and of course the medical team wishes that would happen too,” she said. “But when it gets to the point where clearly that isn’t going to happen, that’s often where I have to reframe the faith stance: The miracle isn’t that my loved one is going to wake up and come back to life again. The miracle is that they will help someone else to do that and not die.”
A sacred circle
That religious and spiritual aspect of organ donation is being recognized this week during National Donor Sabbath – a time when faith leaders from all major religions encourage their congregations to become organ donors.
It’s a once-a-year event for most religious leaders, but it’s a regular occurrence for Stephanie and the team of chaplains at VCU Medical Center.
“Knowing you are helping someone else through the gift of life through organ donation can have a lot of meaning to those going through the grief journey.”
As a chaplain, Stephanie often talks with families about “what comes next” after they’ve accepted that their loved one will not recover.
For many, what comes next is the decision to donate. It helps when families know the wishes of their loved one.
“Knowing you are helping someone else through the gift of life through organ donation can have a lot of meaning to those going through the grief journey. It is the realization that my loved one could help someone. This is their legacy and can really help the bereavement process.”
At VCU Health, it’s the LifeNet representative who usually brings up the subject first. Stephanie then helps to counsel them and talk them through it. While she supports organ donation, her role as a spiritual caregiver is to ensure that the family feels comfortable with whatever decision they’ve made.
“And if this decision is yea or nay, for whatever reason, you want it to be what was right for them so they don’t look back and go ‘God, I wish I had done it differently.’”
“As chaplains, our role is neutral in providing the support and in bringing everyone together,” she said. “You want the family to look back and know they made the right decision. And if this decision is yea or nay, for whatever reason, you want it to be what was right for them so they don’t look back and go ‘God, I wish I had done it differently.’”
Regardless of a family’s decision, Stephanie says she feels privileged to be invited into a sacred circle. “The grief and the joy, the love and the pain, are all interwoven in living and dying. We can’t separate them out.”
Saying no
Sometimes a family decides not to donate because they’ve had too much and they can’t make another decision; they want to just be done and go home. Sometimes there’s a lack of family consensus. Sometimes the family doesn’t trust hospitals or doctors or medicine because of negative past experiences. In those cases, Stephanie works with the team and the family to best coordinate communication and support; helps everyone to process their grief, and to feel as comfortable as possible with their choices.
“As chaplains, our role is neutral in providing the support and in bringing everyone together,” she said. “You want the family to look back and know they made the right decision.”
But sometimes, she said, families initially say they don’t want to donate because of what turns out to be a misconception. For instance, some people are concerned that organ donation will affect funeral arrangements or that their religion may prohibit it.
When that happens, Stephanie, as family communication coordinator ensures the family receives clarifying information; provides a shoulder to cry on, and gently provides the grief support the family needs.
Saying yes
For many families, the end-of-life event is sudden, tragic and unexpected. They’re overwhelmed, shocked and stricken with grief and they can’t think fast enough to process all of the decisions that are flying at them.
For others, it’s a more gradual process. They gather and wait and watch and pray for a miracle.
So for Stephanie, the key is understanding and knowing what to say and when to say it.
“Part of it is timing and knowing, when families are faced with a lot of decision-making, when to introduce this new thing and add it to the mix,” she said.
Sometimes they get there on their own. One family Stephanie remembers had been waiting and holding on, praying for a miracle, unwilling to consider any other possibility. She left them for only a few minutes to go off the unit. When she came back, the nurse had also just paged her to indicate everything had changed – the wife had suddenly decided it was time to turn off her husband’s machines.
Stephanie called for the LifeNet representative, who came and explained the organ donation process. That was all it took.
“The only thing the wife said was ‘He would like that,’” Stephanie said.
The family ended up taking great comfort in the fact that their loved one could help others. For that family and for many others, finding some meaning helped to make the death more bearable.
Finding hope and meaning
“It’s a way to make sense of something that is senseless,” Stephanie said. “It helps give it meaning and also it helps them to not be helpless. It is literally giving someone life. So they can’t change the outcome for their own child or whoever it is, but they can change the outcome for somebody else so it empowers them in the midst of being totally grief-stricken and out of control. It gives them a measure of control to feel “Wow. I have the power to help somebody else and give somebody else life.”
“It’s a way to make sense of something that is senseless.”
Finding meaning in life and in death is part of Stephanie’s own daily goal.
“I have no problem with dying. I would like my dying to be meaningful for others if possible,” she said. “People ask me how I stay vibrant and positive. My positivity comes out of my morbidity. Today could be the last day of my life and if it is, I want it to be meaningful.” To me that’s the bottom line – to live and die meaningfully.”